Viruses armed with the gene-editing tool CRISPR could someday be used to treat urinary tract infections (UTIs), results from an early clinical trial suggest.
However, the experimental treatment, which would be used in tandem with traditional antibiotics, still has more tests to undergo before it could be approved for clinical use.
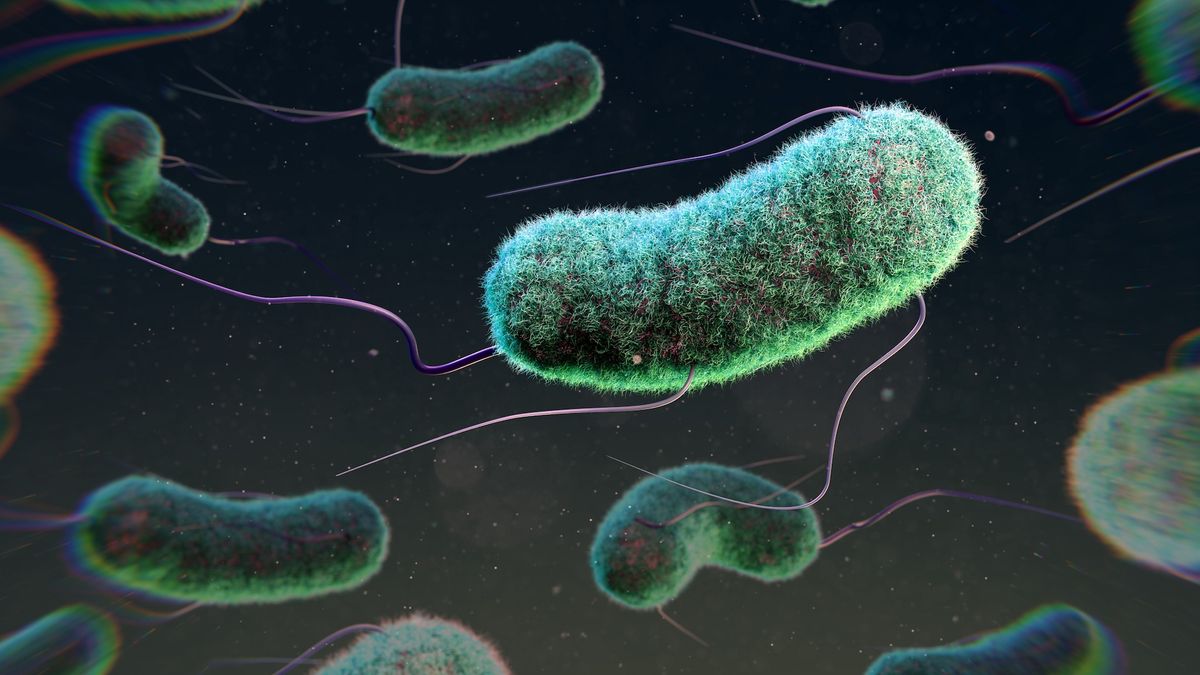
The treatment harnesses bacteriophages, or viruses that infect bacteria. Also called “phages” for short, the viruses are being developed as a potential alternative to conventional antibiotic drugs.
One reason phages are appealing is they can be incredibly selective, taking aim at only specific bacterial strains. This sidesteps problems posed by broader-spectrum antibiotics, which can kill a range of bacteria and thus pressure many microbes to evolve antibiotic resistance. Broad-spectrum antibiotics can also inflict collateral damage on helpful bacteria, including those in the gut microbiome.
Related: Dangerous ‘superbugs’ are a growing threat, and antibiotics can’t stop their rise. What can?
Phages aren’t totally immune to resistance; bacteria can evolve strategies to survive the attack of individual viruses. However, multiple phages can be combined into one treatment, forcing the bacteria into a corner.
That’s the case for LBP-EC01, the new phage therapy being tested for UTIs. Specifically, LBP-EC01 is designed to kill Escherichia coli, the main culprit behind UTIs.
Made by the company Locus Biosciences, the experimental treatment was described in a paper published Aug. 9 in the journal The Lancet Infectious Diseases. LBP-EC01 would be used alongside a traditional antibiotic to boost that antibiotic’s effectiveness and thus reduce the dose needed to cure an infection. (Some other phage therapies are being considered as standalone treatments.)
LBP-EC01 contains six phages, three of which are “lytic,” meaning they invade bacterial cells and split them open. The three remaining phages are engineered to carry genes for a CRISPR system. CRISPR is a precise tool that can be used to cut through specific sequences within DNA. Once it’s inside an E. coli cell, this CRISPR machinery goes after bits of the bacterial genome that are crucial to the microbe’s survival.
“The real draw of it is that it is a sequence-specific tool,” meaning the treatment targets only the DNA you tell it to and not sequences present in other cells, Chase Beisel, co-founder and scientific adviser of Locus Biosciences, told Live Science in 2023. So, once administered to a patient, “the CRISPR machinery gets into a set of cells, but only those that have the sequence or sequences you picked will be attacked and killed,” he explained.
Locus Biosciences has just completed the first part of a two-part trial of LBP-EC01. The treatment is being tested for uncomplicated UTIs, meaning those that don’t involve structural abnormalities in the urinary tract or additional medical problems, such as having a weakened immune system.
The first part of the trial, which included 39 adult female patients, was aimed at identifying a safe dose of the treatment to move into further testing. All of the patients had a history of at least one drug-resistant UTI caused by E. coli in the year prior to the trial.
Tests conducted in the trial ultimately zeroed in on a quick, three-day course of the treatment that’s given alongside an antibiotic called trimethoprim-sulfamethoxazole (common brand name Bactrim). No serious side effects were observed with this dosing regimen. In addition, samples of the patients’ UTI bacteria didn’t show signs of evolving resistance after the treatment.
Related: New UTI vaccine wards off infection for years, early studies suggest
In a subset of 16 patients, the scientists looked more closely at how well the treatment worked against the UTIs. They saw a “rapid reduction of E. coli” in patients’ urine within four hours of the first dose. All 16 patients’ UTI symptoms had completely resolved by the 10th day after starting treatment. By then, 14 of the 16 had low enough E. coli levels in their urine to be considered cured of the infection, as well.
Eleven of these 16 patients were infected by bacteria that were resistant to TMP-SMX at baseline, the study authors noted. That suggests that the phage treatment worked synergistically with the antibiotic, lowering the bacteria’s defenses so even antibiotic-resistant infections could be cleared.
However, because the main goal of this study was to select a dose, not to test the treatment’s efficacy, the second phase of the trial will now compare LBP-EC01 to a placebo. In addition, the first leg of the trial was quite small, the study authors noted, but the next phase will include up to 288 participants.
There’s more work to be done to move LBP-EC01 toward an official approval. However, broadly speaking, “I can see these [types of treatments] coming about in the five- to 10-year time frame,” Beisel previously told Live Science.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to [email protected] with the subject line “Health Desk Q,” and you may see your question answered on the website!